 Sure, this is the fifth post of 2016 – and its July – however there is a good reason for it. I continue to be an on the field athletic trainer, I continue to educate on concussion, I continue to be active on Twitter but more importantly I am concentrating more on being a father and husband. Blogging ain’t easy, folks; let’s be honest the coverage of concussion has blossomed well since 2009 when this blog started.
Sure, this is the fifth post of 2016 – and its July – however there is a good reason for it. I continue to be an on the field athletic trainer, I continue to educate on concussion, I continue to be active on Twitter but more importantly I am concentrating more on being a father and husband. Blogging ain’t easy, folks; let’s be honest the coverage of concussion has blossomed well since 2009 when this blog started.
All of that being said, I am also in the process of gaining further education in concussion. This is not your typical education about the injury but right were my mantra for the past six years has been:
The injury of concussion is not the true problem; it is the mismanagement of this brain injury that is the real issue.
As noted in March I began the Evidence in Motion Concussion Management Course. This is a 34 week program that was designed to bring collaboration and current information to those that can impact the real problem of this injury, the clinicians.
We have arrived at the half way point in the program, marked by the weekend intensive course – which met in Chicago this past weekend. Many have wanted to know has it been worth it. The answer is unequivocally, YES.
Before I get to the hands on of the weekend let me recap the first half of the program. One word cannot do it justice but in our search for snippets of information and quick reaction, that one word could be “trailblazing”.
Previously I wrote about how the program was basically going in terms of mechanics and what we were doing at the time. Since then I have read more research (current), discussed, and most importantly learned how to better help those that have been concussed.
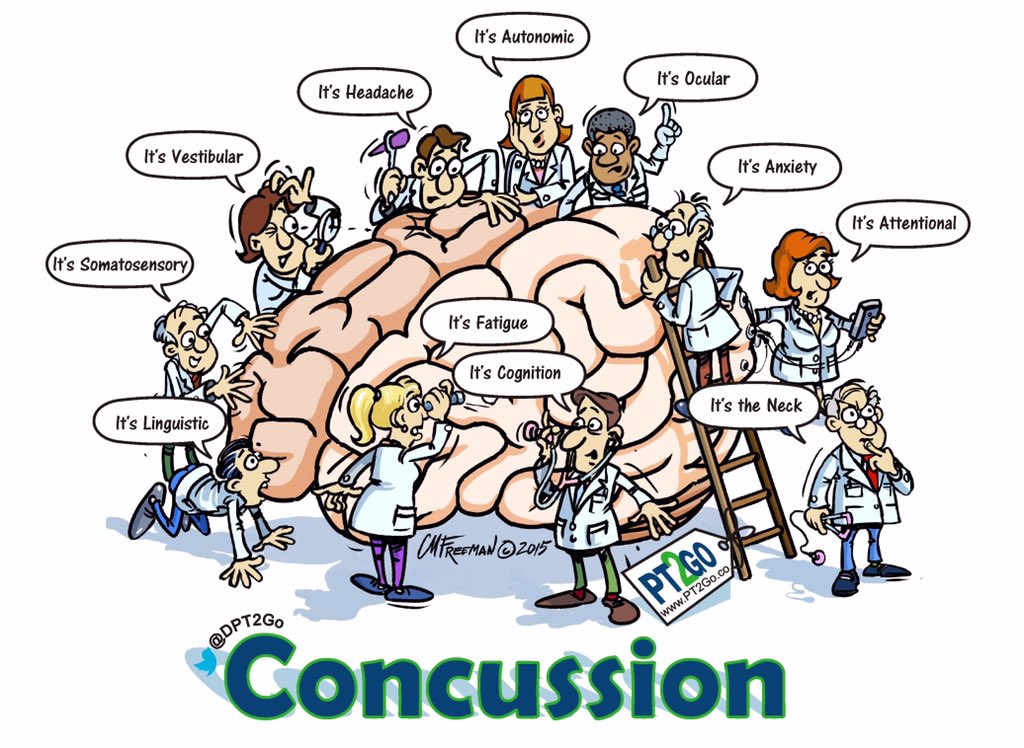
We finished the Therapeutic Neuroscience Education and moved into the specifics of the concussion and its management. We spent a week on each of the following parts of the concussion continuum:
- Emergency Department – evolution and how they view the injury
- Orthopedics – how concussion relates to bones and muscles (neck)
- Vestibular Rehab – not only the vestib system but really focusing on the eyes
- Adult/Migraines – a previously unthought of link/predisposition for concussion
- Vision Rehab – what I feel will be the next area of focus for recovery from concussion
- Neuropsych/Return to Learn – how we all fit together in these areas as clinicians
- Speech Language Pathology – unknown to me how these professionals can and will help
Those seven weeks, plus the last week of summary were probably the most challenging Continue reading
 The meeting at Georgetown University this past weekend was more than fruitful for this athletic trainer. I went in trying to get two things done: one, provide info to you the follower as best as possible and move along the discussion on female concussion and two, to learn something that is applicable to me as a “boot on the ground” athletic trainer.
The meeting at Georgetown University this past weekend was more than fruitful for this athletic trainer. I went in trying to get two things done: one, provide info to you the follower as best as possible and move along the discussion on female concussion and two, to learn something that is applicable to me as a “boot on the ground” athletic trainer. If there has ever been a tenacious and relentless person in the concussion space my observation is that it is this one person. Not a researcher, not a physician, not a policy maker… A mom… Her name Katherine Snedaker.
If there has ever been a tenacious and relentless person in the concussion space my observation is that it is this one person. Not a researcher, not a physician, not a policy maker… A mom… Her name Katherine Snedaker.
 Originally titled
Originally titled  What follows below are recommendations that have been on this blog for many years. I came up with them when it started in 2010 and not much has happened to change what was written. In fact, more and more these ideas have been accepted, showing that it was ahead of its time in 2010.
What follows below are recommendations that have been on this blog for many years. I came up with them when it started in 2010 and not much has happened to change what was written. In fact, more and more these ideas have been accepted, showing that it was ahead of its time in 2010. For those new to the blog, Nick Mercer is our only “staff” writer here at The Concussion Blog. He provides a great layman’s perspective; one from a person recovering from a traumatic brain injury. If you want to know why he does this – for us and himself – you can read
For those new to the blog, Nick Mercer is our only “staff” writer here at The Concussion Blog. He provides a great layman’s perspective; one from a person recovering from a traumatic brain injury. If you want to know why he does this – for us and himself – you can read  Eleven years ago my balance and mobility were better than good. My health was better than good. Ten years and seven months ago, I was a long way away from feeling anything remotely close to good about my balance and my mobility, or about my health at all. That was a drastic turn, and it sucked, but it happened. I can’t pretend it didn’t. Well, I could pretend, but what good would that do?
Eleven years ago my balance and mobility were better than good. My health was better than good. Ten years and seven months ago, I was a long way away from feeling anything remotely close to good about my balance and my mobility, or about my health at all. That was a drastic turn, and it sucked, but it happened. I can’t pretend it didn’t. Well, I could pretend, but what good would that do? Technology is ever-expanding in all areas of our life; in my short time we have gone from land line phones and massive desktop computers that could play “Lemonade Stand” to handheld personal computers that is also a phone. The point being that technology is amazing. In the previous post we discussed how MRI now can actually see damage to the white matter in the brain after concussion. Until that information was presented the changes in the brain were only theorized about.
Technology is ever-expanding in all areas of our life; in my short time we have gone from land line phones and massive desktop computers that could play “Lemonade Stand” to handheld personal computers that is also a phone. The point being that technology is amazing. In the previous post we discussed how MRI now can actually see damage to the white matter in the brain after concussion. Until that information was presented the changes in the brain were only theorized about. OK, that title may be hyperbole, but the new research out of Canada should make you take a step back and realize what our fine researchers are now able to discover. Considering the context of hockey it shouldn’t be shocking that this was found in Canada (since posting we have been informed that work was done on both sides of the border), but really for a long while now some of the best work on concussions is coming from the North, for whatever reason (no disrespect to the US scientists).
OK, that title may be hyperbole, but the new research out of Canada should make you take a step back and realize what our fine researchers are now able to discover. Considering the context of hockey it shouldn’t be shocking that this was found in Canada (since posting we have been informed that work was done on both sides of the border), but really for a long while now some of the best work on concussions is coming from the North, for whatever reason (no disrespect to the US scientists).
 As an athletic trainer – an opinionated one at that – I struggle with all the “bells-and-whistles” in this conundrum that is the concussion issue. If you have visited here or heard me speak you undoubtedly know that mismanagement of concussions is the true issue of this complex paradigm. Yes, we need to know when a concussion occurs to begin the process in the right direction; however, this can be accomplished by simply making sure you have a trained medical professional on hand when the need arises. Getting an athletic trainer to cover the most at risk sports at the most at risk times is a great start (and in the authors opinion is the only choice if you want to have collision sports). Short of that,
As an athletic trainer – an opinionated one at that – I struggle with all the “bells-and-whistles” in this conundrum that is the concussion issue. If you have visited here or heard me speak you undoubtedly know that mismanagement of concussions is the true issue of this complex paradigm. Yes, we need to know when a concussion occurs to begin the process in the right direction; however, this can be accomplished by simply making sure you have a trained medical professional on hand when the need arises. Getting an athletic trainer to cover the most at risk sports at the most at risk times is a great start (and in the authors opinion is the only choice if you want to have collision sports). Short of that,  Concussions have gained so much attention that the news is almost inundated with story-after-story of occurrences, recovery, litigation and people trying to mitigate the injury. There seems to be a shortage of press clipping and stories on how to handle this injury. More often I have witnessed stories downplaying the injury or the oft cited “
Concussions have gained so much attention that the news is almost inundated with story-after-story of occurrences, recovery, litigation and people trying to mitigate the injury. There seems to be a shortage of press clipping and stories on how to handle this injury. More often I have witnessed stories downplaying the injury or the oft cited “ A paramount review of concussions and their “long-term” effects has been published (or soon will) in
A paramount review of concussions and their “long-term” effects has been published (or soon will) in  As has been said countless times in countless articles about brain injury, “every brain injury is different”. I don’t know and don’t care to know how many times I’ve heard or read it. That phrase is used primarily for the benefit the general public to explain or define a lasting injury about which little is known. Although geared towards people who have – seemingly – little or no experience with brain injury, the statement should still be understood as fully as possible by those of use who have such experience.
As has been said countless times in countless articles about brain injury, “every brain injury is different”. I don’t know and don’t care to know how many times I’ve heard or read it. That phrase is used primarily for the benefit the general public to explain or define a lasting injury about which little is known. Although geared towards people who have – seemingly – little or no experience with brain injury, the statement should still be understood as fully as possible by those of use who have such experience. If you all recall I went to Zurich in November to attend the “Concussion Conference”; mainly as an observer, but there was enough time and opportunity to impart my questions/knowledge as a practicing athletic trainer. Here are the links to
If you all recall I went to Zurich in November to attend the “Concussion Conference”; mainly as an observer, but there was enough time and opportunity to impart my questions/knowledge as a practicing athletic trainer. Here are the links to  Certainly the research is flying in; mostly the investigations are now looking at either ways to detect the injury or objective ways to determine recovery. There are a bunch of other designs and angles out there but the most important are the above. Although it would be great if we had an objective way of determining concussion, it is really not the pressing issue (with solid education and conservative approach to injury – sit them out).
Certainly the research is flying in; mostly the investigations are now looking at either ways to detect the injury or objective ways to determine recovery. There are a bunch of other designs and angles out there but the most important are the above. Although it would be great if we had an objective way of determining concussion, it is really not the pressing issue (with solid education and conservative approach to injury – sit them out).

 I received the following press release about a Concussion Symposium coming up in March. The faculty is not your “usual suspects” rather some very good and known people in the medical field. If you get the chance to head down to Texas for that Saturday I believe you will not be wasting your time or resources. I would love to make it, however I have a prior commitment; that being said someone take good notes for me.
I received the following press release about a Concussion Symposium coming up in March. The faculty is not your “usual suspects” rather some very good and known people in the medical field. If you get the chance to head down to Texas for that Saturday I believe you will not be wasting your time or resources. I would love to make it, however I have a prior commitment; that being said someone take good notes for me.
